While there is an estimated 1 in 10 women diagnosed with endometriosis, one third of that group will have endometrial tissue on their bowel. This means that the endometrial tissue grows on the surface or even inside of your intestines. I am part of this unfortunate group of bowel endo patients. My symptoms were originally misdiagnosed as Crohn’s and then Irritable Bowel Syndrome (IBS). I would fluctuate between constipation and diarrhea without warning. In addition, I suffered severe abdominal cramping, bloating, fatigue and nausea. Many doctors told me it was the food I was eating causing these issues, so I changed everything I ate and began to eat healthier. This made everything worse. I was exercising and eating healthier, but I was getting worse. This didn’t make sense to me. My local doctors didn’t understand what was happening either. It wasn’t until I saw my gynecologist that she said she thought it might be related to my endometriosis. I had already had a full hysterectomy, but apparently endo had already infiltrated my digestive tract and was wreaking havoc. This was evident by the MRI that was ordered. Pictured below is the large endometrioma measuring an estimated 7 cm in diameter that had grown within my bowel walls, causing a nearly 100% blockage. This was the source of my pain and cycling constipation and diarrhea. Not only was my endo surgeon concerned about the size of this endometrioma, she didn’t routinely treat bowel endo which meant we needed to call in a colorectal endometriosis specialist to consult on my case.
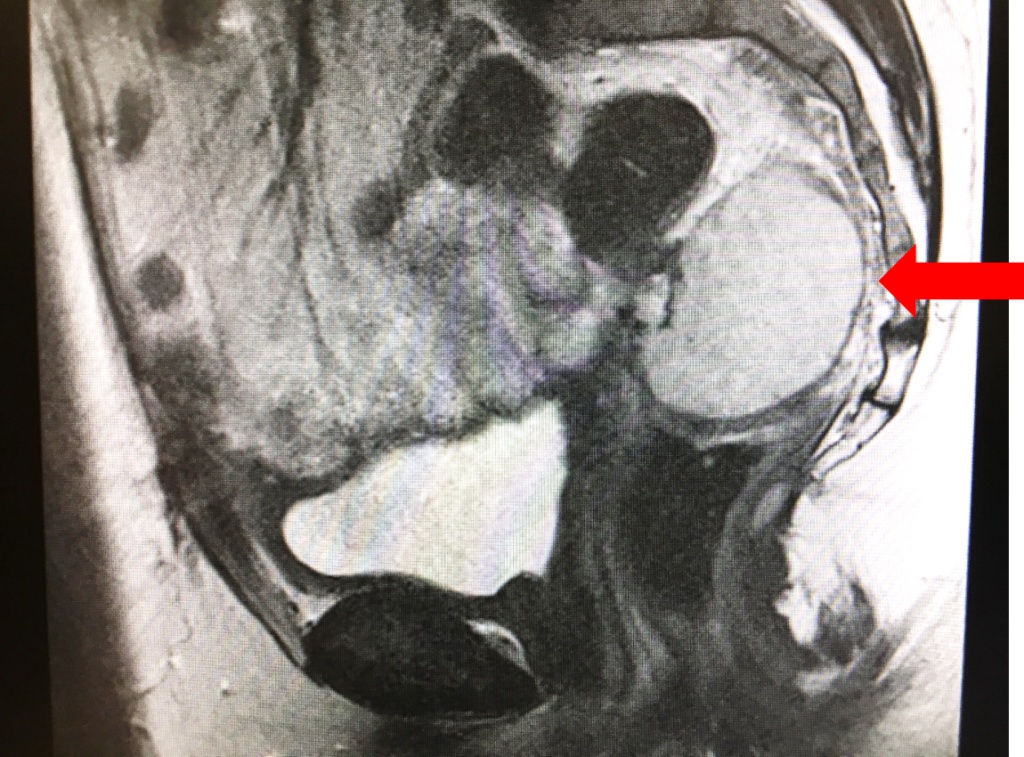
This new specialist reads the scans and lab reports and starts throwing terms out like bowel resection, loop ileostomy, external intestine, soft GI diet….to the point where I think I start to black out. Woah, what just happened? I looked at the scan and what appeared to be an Ostrich egg within my bowels and next thing we know he’s talking about taking it all out. So I look blankly at him and say, OK, I think I blacked out, start this again in lay terms for me as this is a new endo thing I haven’t heard about. He starts again and tells me that he needs to remove my “egg” which means taking out that section of the bowel and to allow this area to heal we would need to divert digestive matter elsewhere. Upon removal of the bad area, he would then reconnect the 2 good sections together to allow a complete connection. OK, I get it now, so where is “elsewhere”? He then proceeds to tell me he’s going to pull a part of my intestine through my belly and stitch it in place so that all poop can come out there into a bag which I would need to care for. At this point, I think I was in too much shock to comprehend what all this would entail and just wanted to cry. He says he hopes that everything would heal in a few months and then we can stuff the small intestine back in and reverse everything. So what I heard was that this is NOT a permanent fixture and we can reverse this. OK – that was somewhat comforting, but still stress inducing.
It’s taken a few weeks to get everything scheduled and researched so that I’m more comfortable with the procedure and associated terminology, but if this is what it will entail to get rid of this endometrioma (Ostrich egg), I’m game. Bowel endo is not for the faint of heart, to say the least. Be glad that there is only a small portion of the population that is affected with this horrible form of severe endometriosis.
** Spam comments from non verified users will not be approved.**